Dysmenorrhoea: Causes, Symptoms, Types, and Natural Relief Tips

Dysmenorrhoea may be the medical term, but the experience is familiar to many: period pain that isn’t just uncomfortable, but draining, distracting, and capable of throwing an entire day off course. What makes dysmenorrhoea different from regular cramps is not just the pain itself, but its pattern, intensity, and how deeply it affects daily functioning. For some, it's a monthly inconvenience. For others, it can feel like a cycle of pain that keeps returning stronger. Understanding what’s actually going on inside the body is the first step to managing it better.
Why Does Dysmenorrhoea Happen?
The uterus contracts throughout menstruation to shed its lining. These contractions are controlled by prostaglandins - the chemicals that rise just before the period begins. Higher prostaglandin levels lead to stronger, sharper contractions and temporarily reduced blood flow to the uterus, causing pain.
In dysmenorrhoea, this pain is amplified because prostaglandin production is higher, pain pathways are more sensitised, or an underlying condition is making the uterus react more intensely. This is why dysmenorrhoea often feels deeper, more persistent, and more overwhelming than ordinary cramps.
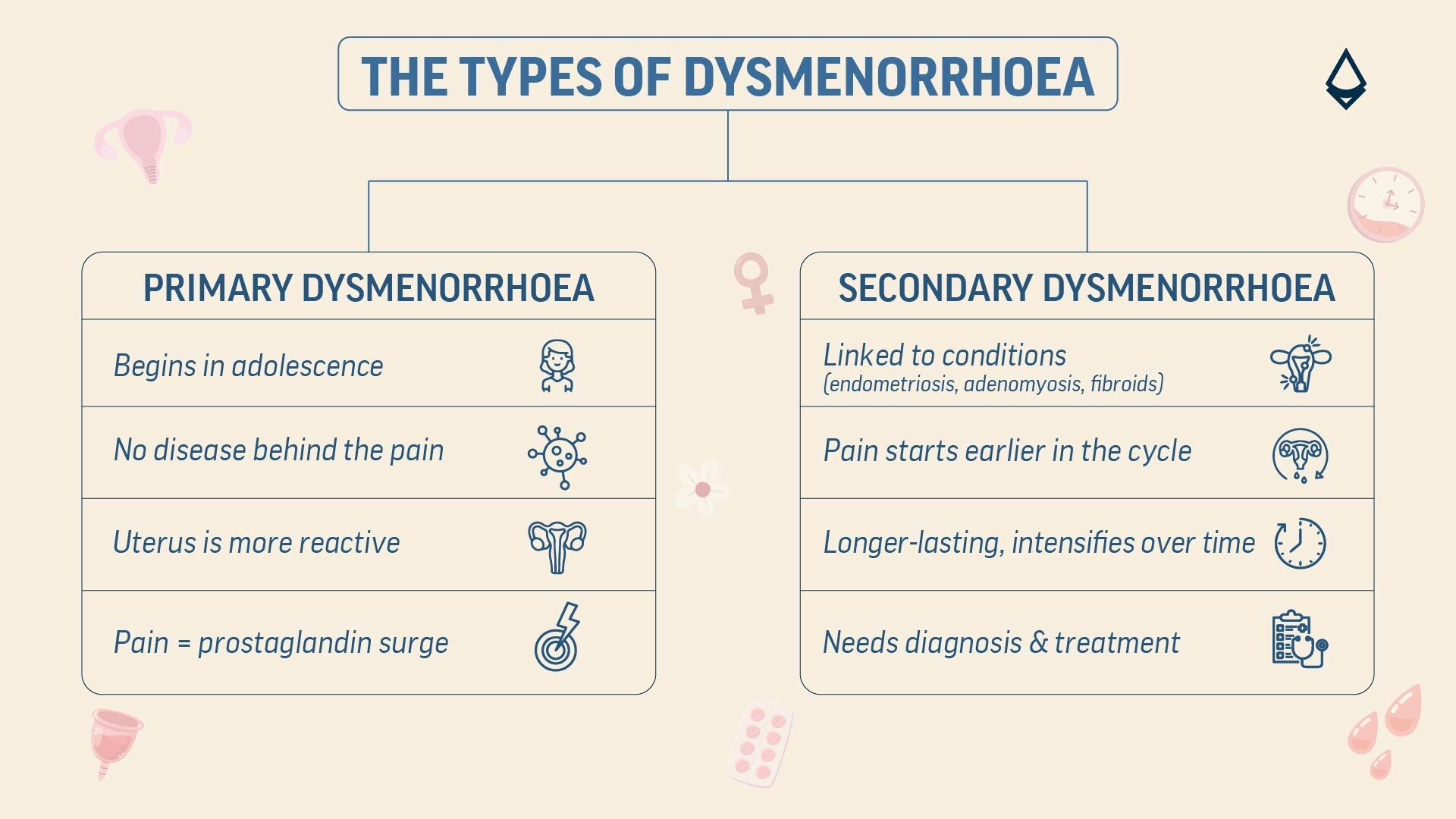
Primary vs Secondary Dysmenorrhoea
Dysmenorrhoea isn’t one single condition; its cause determines its type:
Primary dysmenorrhoea usually starts in the teenage years and is linked to excess prostaglandins. There’s no underlying disease; the uterus is simply more reactive.
Secondary dysmenorrhoea is caused by another health condition. Endometriosis, adenomyosis, uterine fibroids, pelvic inflammatory disease, and cervical stenosis are common culprits. Here, the pain may worsen with age, last longer, or occur even before periods begin.
The key difference is that primary dysmenorrhoea is functional; secondary dysmenorrhoea is symptomatic of something deeper.
Symptoms that Point to Dysmenorrhoea
While abdominal cramps are the most obvious sign, dysmenorrhoea often comes with a cluster of symptoms because prostaglandins don’t just act on the uterus; they affect the whole system.
Common symptoms include:
Nausea or vomiting
Diarrhoea
Lower back or thigh pain
Headache
Bloating
Dizziness
Extreme fatigue or weakness
These symptoms are often strongest in the first 24 to 48 hours of bleeding, but many women notice them just before their period begins.
Who Is More Likely to Experience It?
Certain factors increase the chances of dysmenorrhoea being more severe or long-lasting:
Early onset of menstruation
Heavy or prolonged bleeding
Irregular cycles
Smoking
High stress levels
Very low physical activity
Family history of painful periods
Conditions like PCOS, endometriosis, or fibroids
Even long sitting hours, poor sleep, and inflammatory diets can make symptoms flare.
When Is It Time to Seek Medical Help?
Dysmenorrhoea deserves attention when pain stops being predictable or manageable. Warning signs include:
Pain that suddenly becomes more severe than previous cycles
Pain lasting beyond three days
Pain that disrupts work, sleep, or everyday tasks
Very heavy bleeding or passing large clots
Pain during urination or intercourse
Fever, nausea, or vomiting that feels unusual
Rapidly worsening symptoms over months
These signs often indicate secondary dysmenorrhoea and should be evaluated early to prevent long-term complications.
Why Stress Makes It Worse?
Stress hormones like cortisol interfere with the delicate hormonal rhythm of the menstrual cycle. High stress increases inflammation, tightens muscles, and heightens pain signals. Short relaxation practices, breathwork, or even stepping away from screens before bedtime can help regulate pain perception over time.
Holistic Approaches for Easing Dysmenorrhoea
Dysmenorrhoea often responds best to a combination of gentle, consistent habits that calm inflammation, relax pelvic muscles, and support hormonal balance. Warmth remains a reliable first step as heat softens tight uterine muscles and improves blood flow, which naturally reduces cramp intensity. Slow, steady movement, such as light yoga, walking, or mobility exercises, helps the pelvis stay open and lowers the sensitivity of pain pathways.
Nutritionally, the focus shifts to foods that tame inflammation and support muscle relaxation. Magnesium-rich seeds and nuts, omega-3 sources like walnuts or flaxseeds, and spices such as ginger and turmeric help regulate prostaglandin activity and smoothen uterine contractions. Hydration plays an underrated role, too.
Other than these, cannabinoid-based medication offers an additional natural route. By interacting with the body’s endocannabinoid system, cannabinoids help modulate pain signals, relax smooth muscles, and reduce inflammation, making them a plant-derived option for those seeking more sustained relief alongside lifestyle strategies.
Conclusion
Dysmenorrhoea is more than just painful periods. Paying attention to patterns, like when the pain starts, what worsens it, and which symptoms accompany it, can help us understand our body better. If the pain suddenly intensifies, starts earlier than usual, or begins to interfere with daily routine, it’s important not to ignore it. Speaking to a gynaecologist for timely evaluation and guidance can help manage the pain effectively and prevent it from becoming a long-term struggle.
Read more:
Key Takeaways
- - Dysmenorrhoea is severe period pain caused by high levels of prostaglandins, which trigger intense uterine contractions and reduced blood flow.
- - It is categorized into two types: Primary (functional cycle pain) and Secondary (pain caused by underlying issues like fibroids or endometriosis).
- - Symptoms often affect the whole body, leading to nausea, headaches, and fatigue because the chemicals involved travel through the entire system.
- - Management focuses on relaxing pelvic muscles through heat therapy, magnesium-rich nutrition, and gentle movement to lower inflammation.